Red Light Therapy for Acne: What the Clinical Evidence Shows (and Who It’s Best For)
Red light therapy supports skin repair and inflammatory balance at a cellular level, helping acne-prone skin recover more effectively over time.
Acne is not just a surface-level skin issue. It’s a complex inflammatory condition influenced by bacteria, hormonal signalling, immune response and skin barrier health. While topical treatments and prescription medications can play a role, many people are now looking for non-invasive, evidence-led ways to support acne-prone skin without irritation or long-term side effects.
Red light therapy - often used alongside blue light — has emerged as one of the most researched light-based approaches for acne management. But what does the science actually say, and who is it most suitable for?
This guide breaks down the research, the mechanisms involved, and how red and blue light therapy are used in practice to support acne-prone and inflamed skin.
How Acne Develops (Beyond Blocked Pores)
Bacterial Overgrowth and Acne-Causing Microbes
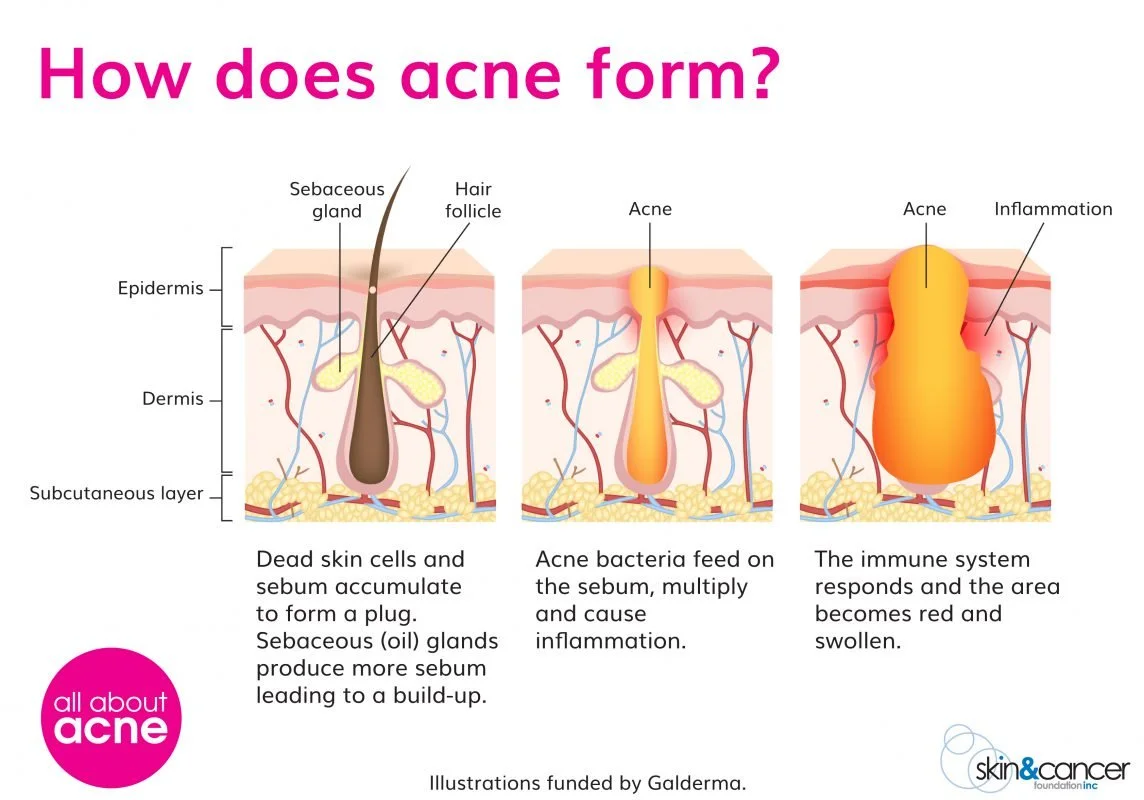
One of the most well-known contributors to acne is the overgrowth of Cutibacterium acnes (formerly Propionibacterium acnes), a naturally occurring bacterium within the skin microbiome. When excess sebum and dead skin cells accumulate within the follicle, they create an environment where C. acnes can proliferate.
As these bacteria break down sebum, they release inflammatory by-products that trigger an immune response — contributing to redness, swelling and painful inflammatory lesions. This is why acne is now classified as both a microbial and inflammatory condition, rather than a purely cosmetic concern.
Inflammation: The Core Driver of Acne Severity
Inflammation plays a central role at every stage of acne development. Even early-stage breakouts often show signs of subclinical inflammation before visible spots appear. Once inflammation is activated, it amplifies redness, prolongs healing time and increases the risk of post-inflammatory marks.
This inflammatory response explains why many acne treatments that aggressively strip the skin can make symptoms worse. When the skin barrier is compromised, inflammatory signalling increases - often leading to more frequent or persistent breakouts rather than resolution.
Inflammatory acne often affects the jawline and cheeks, driven by a combination of bacteria, inflammation and hormonal signalling beneath the skin.
Sebum Production and Follicular Dysfunction
Sebum is essential for skin health, but altered or excessive sebum production can contribute to acne-prone skin. Hormonal fluctuations - particularly involving androgens - influence sebaceous gland activity, increasing oil production within the follicle.
When sebum becomes trapped alongside dead skin cells, it disrupts normal follicular function. This creates microcomedones, the earliest precursor to acne lesions, which can progress into inflammatory papules, pustules or cystic breakouts.
Skin Barrier Disruption and Acne-Prone Skin
A healthy skin barrier plays a crucial role in regulating inflammation and protecting against environmental stressors. In acne-prone skin, the barrier is often compromised — either as a result of the condition itself or from overuse of harsh topical treatments.
Barrier disruption leads to increased water loss, heightened sensitivity and greater inflammatory signalling. This creates a cycle where the skin becomes more reactive, less resilient and slower to heal, increasing the likelihood of recurrent breakouts.
Hormonal and Stress-Related Signalling
Hormonal acne is influenced by fluctuations in cortisol, insulin and androgen activity, which affect both inflammation and sebum production. Chronic stress further compounds this by increasing systemic inflammatory markers and altering immune responses within the skin.
This is why acne often worsens during periods of stress, poor sleep or hormonal change — and why addressing systemic inflammation and recovery is increasingly recognised as part of effective acne management.
Why Treating Acne Requires More Than Surface-Level Solutions
Because acne is driven by bacterial activity, inflammation, barrier dysfunction and hormonal signalling, surface-level treatments alone rarely address the full picture. Approaches that support inflammation regulation, cellular repair and skin resilience are now considered essential alongside topical care.
This broader understanding is why therapies that support the skin at a cellular and inflammatory level, such as light-based photobiomodulation, are increasingly explored as part of evidence-led acne support strategies.
Acne develops when excess sebum and dead skin cells block the hair follicle, allowing acne-causing bacteria to multiply and trigger inflammation beneath the skin.
How Light Therapy Interacts With Acne-Prone Skin
Light therapy works through photobiomodulation, where specific wavelengths of light interact with cellular processes in the skin.
Blue Light and Acne-Causing Bacteria
Blue light therapy (typically around 465 nm) has been widely studied for its ability to target Cutibacterium acnes, the bacteria closely associated with inflammatory acne. These bacteria naturally produce compounds called porphyrins, which absorb blue light energy.
When exposed to blue light, these porphyrins generate reactive oxygen species that damage the bacteria from within, reducing bacterial load inside the follicle without harming surrounding skin tissue. This mechanism is highly specific, which is why blue light is often described as a non-antibiotic approach to managing acne-causing bacteria.
Blue light therapy targets acne-causing bacteria within the skin, helping to reduce active breakouts without antibiotics or harsh topical treatments.
Because of this targeted action, blue light therapy is particularly useful for:
Active breakouts and inflamed acne lesions
Congested or bacteria-driven acne
Skin prone to frequent flare-ups
Importantly, blue light does not rely on antibiotics or harsh topical agents, making it a valuable option for people looking to reduce bacterial involvement in acne without contributing to antibiotic resistance. This is why blue light therapy continues to feature prominently in dermatology research and evidence-led acne protocols.
Red Light and Inflammatory Control
Red light therapy (typically 630–640 nm) works differently to blue light. Rather than targeting acne-causing bacteria directly, red light supports the skin’s inflammatory balance, circulation and repair processes — all of which play a major role in acne severity and healing time.
At a cellular level, red light interacts with mitochondria, helping to optimise cellular energy production (ATP) and support normal tissue function. This is particularly relevant for acne-prone skin, where inflammation often delays healing and increases the risk of persistent or painful lesions.
Research suggests red light therapy may help to:
Reduce inflammatory signalling within the skin
Support cellular energy and repair pathways
Improve circulation and oxygen delivery to affected tissue
Aid recovery of inflamed or damaged skin
For acne-prone skin, this matters because inflammation is often what turns a minor follicular blockage into a larger, more painful breakout. By supporting the skin’s ability to regulate inflammation and repair itself, red light therapy is commonly used alongside blue light as part of a combined, evidence-led acne support approach.
Full-body red light therapy using NovoTHOR supports cellular repair, circulation and inflammatory balance, which can indirectly benefit acne-prone skin.
Why Combining Blue and Red Light Matters
Clinical studies consistently show that combined blue-red LED protocols outperform single-wavelength treatments for acne.
Blue light addresses the bacterial component, while red light supports:
Reduced redness and swelling
Faster lesion healing
Improved skin tolerance
Lower risk of post-inflammatory marks
In clinical trials, combined protocols have reported 46–81% reductions in acne lesions over 8–12 weeks, depending on severity and treatment frequency.
Acne Isn’t Always Just a Skin Issue
Many people experience acne that flares alongside:
Hormonal changes
Chronic stress
Systemic inflammation
Poor sleep or recovery
This is where whole-body photobiomodulation can play a supportive role.
At ReGen Rooms, targeted facial LED treatments are often complemented by NovoTHOR full-body red light therapy, which supports systemic inflammation control, circulation and recovery - all of which influence skin health indirectly.
You can read more about how photobiomodulation supports skin health more broadly in our guide:
Who Red Light Therapy for Acne Is Best Suited For
Light-based therapy is commonly used by people who:
Experience inflammatory or hormonal acne
Have acne-prone skin that reacts poorly to harsh topicals
Want to reduce reliance on long-term antibiotics
Are managing post-treatment skin recovery
Want a preventative, maintenance-based approach
It’s also frequently used alongside professional skincare and lifestyle interventions, rather than as a standalone “quick fix”.
What a Typical Acne-Focused Light Therapy Protocol Looks Like
Light therapy protocols for acne are always tailored to the individual, but most evidence-led approaches follow a consistent structure designed to address both bacterial activity and inflammation over time.
Targeted Facial LED (Blue + Red Light)
Targeted facial LED treatments combine blue and red wavelengths to address multiple drivers of acne in the same session. Blue light focuses on reducing acne-causing bacteria within the follicle, while red light supports inflammatory balance and skin recovery.
Typical protocols involve:
Frequency: 2 sessions per week
Session time: Approximately 25 minutes
Duration: A minimum of 6–8 weeks
This frequency allows the skin to respond gradually, supporting calmer breakouts, improved healing and better tolerance compared to aggressive topical treatments.
Optional Whole-Body Red Light Therapy (NovoTHOR)
For some people, acne flare-ups are closely linked to stress, hormonal changes or systemic inflammation. In these cases, whole-body red light therapy may be used alongside facial treatments to support skin health more broadly.
Typical use involves:
Frequency: 1 session per week
Particularly beneficial during periods of increased stress or hormonal fluctuation
By supporting circulation, cellular energy and inflammation balance at a whole-body level, this approach can complement targeted facial treatments, especially for adult or stress-related acne patterns.
Why Consistency Matters
Light therapy works by influencing cellular processes rather than forcing rapid surface changes. Because of this, results are cumulative rather than instant. Regular sessions over several weeks allow the skin time to respond, repair and rebalance, which is why consistency is a key part of any acne-focused light therapy plan.
Is Red Light Therapy Safe for Acne-Prone Skin?
When delivered using clinical-grade devices and appropriate protocols, red and blue light therapy are considered low-risk and non-thermal.
Sessions are:
Non-invasive
UV-free
Painless
Suitable for regular use
This is why light therapy is often described as a supportive skin optimisation tool, rather than a medical acne treatment.
Red Light Therapy as Part of a Bigger Skin Strategy
Acne is rarely caused by a single factor. Light therapy works best when combined with:
Barrier-supportive skincare
Nutrition and lifestyle support
Professional guidance
Used this way, it becomes part of a longer-term strategy focused on skin resilience, not just breakout suppression.
Frequently Asked Questions
-
Blue light therapy has been shown to target Cutibacterium acnes, the bacteria associated with inflammatory acne. The bacteria produce porphyrins that absorb blue light, triggering reactions that damage the bacteria from within, helping to reduce bacterial load without antibiotics.
-
Red light therapy does not target acne bacteria directly, but it supports inflammation regulation, circulation and skin repair. This is important for acne-prone skin, as inflammation often drives redness, swelling and prolonged healing of breakouts.
-
Red and blue light work best together. Blue light helps reduce acne-causing bacteria, while red light supports inflammatory balance and recovery. Clinical studies consistently show improved outcomes when both wavelengths are used in combination.
-
Some people notice calmer skin within a few weeks, but clinical studies typically assess results over 6–12 weeks. Because light therapy works at a cellular level, consistent sessions are important for sustained improvement.
-
When delivered using clinical-grade devices and appropriate protocols, red and blue light therapy are considered low-risk, non-thermal and UV-free. Sessions are non-invasive and commonly used as part of ongoing skin support routines.
-
Yes. Red and blue light therapy are often used to support adult and hormonally influenced acne, particularly where inflammation, stress or delayed healing are contributing factors.
-
No. Light therapy works alongside skincare and professional guidance. It supports skin function and inflammation balance but does not replace cleansing, barrier repair or medical advice when required.
References & Further Reading
Gold, M. H., et al. (2009). Combined blue (415 nm) and red (633 nm) LED phototherapy in the treatment of acne vulgaris.
Journal of Cosmetic and Laser Therapy, 11(2), 86–90.
— Demonstrated significant reductions in inflammatory acne lesions using combined blue and red LED therapy over 12 weeks.Papageorgiou, P., Katsambas, A., & Chu, A. (2000). Phototherapy with blue (415 nm) and red (660 nm) light in the treatment of acne vulgaris. British Journal of Dermatology, 142(5), 973–978.
— One of the earliest controlled studies showing improved acne outcomes with dual-wavelength LED therapy.Lee, S. Y., et al. (2007). A prospective, randomised, placebo-controlled, double-blinded study on the effects of 830 nm LED phototherapy on acne vulgaris. Journal of Investigative Dermatology, 127(1), 1–8. — Supports the role of near-infrared light in reducing inflammation and supporting skin repair.
Avci, P., et al. (2013). Low-level laser (light) therapy (LLLT) in skin: stimulating, healing, restoring. Seminars in Cutaneous Medicine and Surgery, 32(1), 41–52. — Comprehensive review explaining how photobiomodulation affects inflammation, circulation and cellular energy in the skin.
Barolet, D., & Boucher, A. (2010). Prophylactic low-level light therapy for the treatment of hypertrophic scars and skin inflammation. Lasers in Surgery and Medicine, 42(6), 597–601. — Explores anti-inflammatory effects of red and near-infrared light relevant to acne-prone and post-inflammatory skin.
Hamblin, M. R. (2017). Mechanisms and applications of the anti-inflammatory effects of photobiomodulation.
AIMS Biophysics, 4(3), 337–361. — Widely cited paper detailing how red and near-infrared light modulate inflammatory pathways at a cellular level.Fitzpatrick, R. E., et al. (2005). Controlled study of LED phototherapy for skin rejuvenation and inflammation reduction.
Journal of Cosmetic Dermatology, 4(4), 1–7. — Supports broader skin benefits of LED therapy including tone, texture and inflammatory balance.
The information provided is for educational purposes only and does not replace professional medical advice. Individual responses to light therapy may vary.